What Is COPD?
Chronic Obstructive Pulmonary Disease, or COPD, is a long-term illness that impacts how well the lungs function, causing persistent breathing difficulties. It is a broad term encompassing conditions such as chronic bronchitis and emphysema, which restrict airflow and make it challenging to carry out everyday tasks. According to the Centers for Disease Control and Prevention, millions of people in the United States live with COPD, making it the third leading cause of death caused by chronic disease. With no cure currently available, many individuals strive to learn more about their condition and consider enrolling in emerging COPD trials that are studying new therapies or approaches.
Early signs of COPD — such as ongoing cough, wheezing, and frequent respiratory infections — are often overlooked or mistaken for other conditions. However, timely recognition and intervention can lead to a higher quality of life and may even slow the progression of symptoms. Being proactive about lung health equips people with the knowledge to make meaningful lifestyle adjustments, empowering them to manage their condition better and maintain an active role in daily life.
Everyday Challenges Faced by COPD Patients
Tasks that once seemed routine—walking from one room to another, taking a shower, or climbing a few steps—can become physically taxing for individuals living with COPD. Many find themselves frequently out of breath or experiencing fatigue, which may deter them from participating in once-loved activities. The potential for flare-ups, also called exacerbations, adds a layer of unpredictability; these episodes, triggered by respiratory infections or environmental irritants, can be frightening and require immediate action.
Living with this uncertainty causes some people to limit their activities or withdraw from social situations, fearing they might become short of breath in public or need help unexpectedly. Adjustments in routine, pacing tasks, and developing a personal action plan all help restore a sense of control. Individuals often discover new ways to enjoy life while safeguarding their well-being by setting realistic, manageable goals.
Simple Adjustments for Easier Breathing
Make small adjustments at home or work to improve comfort for people with COPD. Position commonly used items within arm’s reach, create clear walkway paths, use lightweight tools, install grab bars for stability, invest in air purifiers or indoor air quality monitors, limit exposure to cigarette smoke, chemical fumes, and heavily scented cleaning products, and practice breathing techniques like pursed-lip breathing. These small adjustments can significantly improve the comfort and independence of individuals with COPD. These changes can save energy, reduce unnecessary movements, and reduce the risk of falls. Regular practice of these techniques can also improve oxygen levels and boost confidence in handling daily situations. These minor adjustments can transform how individuals with COPD interact with their environment and sense of independence.
Importance of Regular Activity and Movement
Regular physical activity is crucial for people with COPD, as it improves lung function and muscle tone and reduces hospitalization risk. Exercise can be light walking, slow cycling, swimming, or seated exercises for those who tire quickly. To ensure safe exercise, consult a healthcare provider or physical therapist, warm up with gentle stretching, and start with manageable sessions. Use assistive devices or supports as needed to prevent falls and maintain balance. Take frequent breaks and listen to your body’s signals. Regular movement supports mental well-being and physical health, releasing endorphins, uplifting mood, and reducing stress. Short movement intervals throughout the day, such as standing and stretching during commercial breaks or gentle walking around the home, keep the body engaged and spirits high.
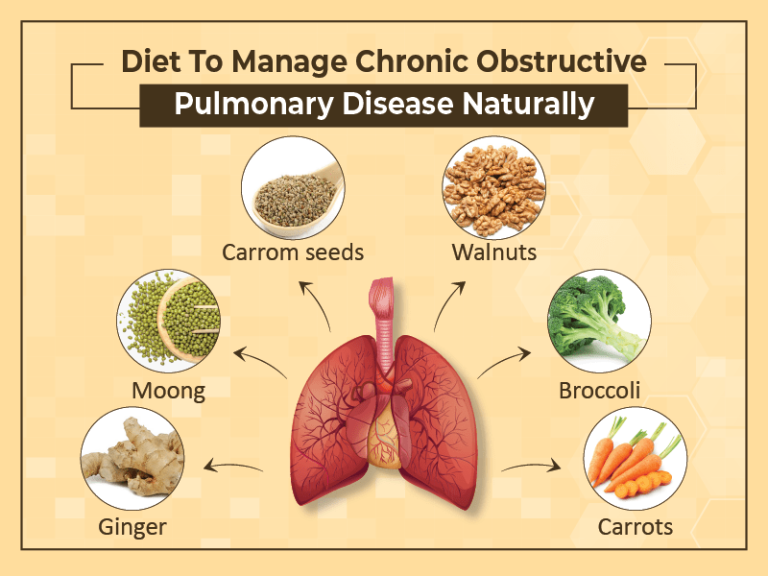
Healthy Eating Tips for COPD
Nutrition is crucial for managing COPD symptoms and overall health. Heavy, rich meals can cause discomfort and difficulty breathing. Experts recommend eating smaller, nutrient-dense meals more frequently for better digestion and energy balance. Choose lean meats, fish, beans, and wholesome grains for protein and healthy muscles. Drink plenty of fluids to keep the mucus loose and easier to clear. Reduce salt intake to avoid swelling in hands, feet, or ankles. Fill your plate with colorful vegetables and fruits for antioxidants, vitamins, and immune function. Preparing meals in advance and storing single-serving portions in the freezer can help on low-energy days. Consult a dietitian or nutritionist to ensure a personalized dietary plan.
Managing Emotional Well-Being
The emotional toll of a chronic condition like COPD should never be underestimated. It is common for people to experience sadness, frustration, or anxiety tied to changing abilities or health setbacks. Constantly navigating limitations—both seen and unseen—can create a persistent strain on self-esteem and motivation.
Finding healthy outlets for emotions can make a noticeable difference in daily mood and resilience. Engaging in relaxing activities, from meditation and reading to sketching and gardening, helps distract the mind from worries. Connecting with a licensed therapist, social worker, or group counselor provides a space to talk openly and learn new coping skills. Social ties are also protective—family, friends, or neighbors who check in regularly help anyone feel remembered and valued.
Building a Support System
Strengthening your support network is empowering and practical, especially when living with COPD. Support groups provide community and connection, offering firsthand experiences, advice, and encouragement. Look for reputable local or national groups dedicated to lung health and chronic respiratory diseases. Ask family and caregivers to learn about COPD and assist with medical appointments, daily chores, and medication management. Communicate your needs, abilities, and boundaries openly to ensure loved ones understand how to provide meaningful support. Prepare an emergency action plan and share it with those closest to you. Support networks nurture hope, build confidence, and remind everyone involved of their support.